There are data about the first person who can be considered cured of HIV without a bone marrow transplant.
A Brazilian man diagnosed with HIV in 2012 maintained a completely suppressed viral load for more than a year after receiving a one-year enhanced treatment regimen, and then stopped taking antiretroviral drugs (ARVs). The researchers pointed out that if enough time passes and a person's viral load does not recover, he may become the first person officially cured of HIV without a bone marrow transplant.
Ricardo Sobi Diaz, MD, PhD, Federal University of Sao Paulo, presented the results of this case study on Tuesday at the International AIDS Conference (AIDS 2020), which is taking place this week.
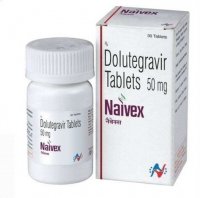
The 35-year-old Brazilian is one of 30 participants in a study of an enhanced treatment regimen, in which the ARV drugs Tivicay (dolutegravir) and Selcentri (maraviroc) were added to the existing HIV treatment regimens of participants together with the drug nicotinamide. The latter drug suppresses the depletion of the immune system and prevents the transition of cells into a latent or non-reproducible state.
The main reason why HIV remains so difficult to treat is that it infects long-lived cells that go into a latent state. ARV drugs work by interrupting various stages of the virus' life cycle in the cell. Therefore, when the cell harboring the virus does not produce new copies, it remains under the radar of standard HIV treatment.
Only one person has been officially cured of HIV: Timothy Ray Brown, an American who was known as the ”Berlin Patient" when his treatment was first published in 2008.
The second person who was probably cured: Adam Castillejo, is known as the “London Patient". Castillejo has not taken ARV drugs for almost three years and his viral load has recovered, according to an update presented at the 2020 conference on Retroviruses and Opportunistic infections in March. But before researchers can be sure that he has really recovered from HIV, additional observations are needed.
Timothy Ray Brown, aka the Berlin patient, watches as Ravindra K. Gupta presents the results of a new case of a probable cure for HIV at CROI 2019.
Both Brown and Castillejo received bone marrow transplants to treat blood cancer. Each of them was compared with a donor who had a genetic anomaly that gives rise to immune cells resistant to HIV.
Adam Castillejo / Facebook
Each of these two cases caused widespread excitement and, at least in Brown's case, served as proof that HIV can be cured. However, relying on bone marrow transplantation to treat the virus is still impractical. This procedure is too dangerous to be ethical for use among people who are otherwise not at risk of death from cancer.
And that's why researchers around the world continue to look for HIV treatments that will prove safe, tolerable, effective and scalable for widespread use.
The Brazilian man in question is a participant in a study in which HIV-positive men aged 18 to 65 years were recruited who, prior to enrollment, maintained a completely suppressed viral load due to ARV treatment and whose lowest CD4 count in history exceeded 350.
During the study, the original ARV regimen for men was supplemented with 50 milligrams of Tivicai once a day plus Selcentri and 500 mg of nicotinamide, each of which was taken twice a day. The men continued this combination treatment for 48 weeks before returning to their original ARV regimen.
On October 12, 2012, the Brazilian was diagnosed with HIV. His viral load before treatment was 20,221.
He started taking the ARV drugs zidovudine (AZT), lamivudine (3TC) and efavirenz on December 11, 2012. In 2014, he switched to efavirenz, lamivudine and Tenofovir disoproxil fumarate (TDF). He has never experienced virological insufficiency, and he has never interrupted his ARV treatment. His lowest CD4 score was 372.
When he entered the study in September 2015, the man's CD4 count was 720. After he started an intensive treatment regimen, he experienced two so—called viral bursts, or moderate, temporary increases in viral load-once at week 16, when he had a very low viral load that did not reach 40, and once at week 24, when he had there was a viral load of 56. Otherwise, routine tests have shown that his virus remains completely suppressed.
The man was present at all planned subsequent visits.
In September 2016, at the end of a 48-week intensive treatment period, the man was removed from Tivicai, Selcentri and nicotinamide, but remained on lamivudine and TDF. He switched to lamivudine, TDF and Viramun (nevirapin) on April 4, 2018, and then to lamivudine, TDF and Tivikai on April 24, 2018.
On March 28, 2019, the man was transferred to analytical treatment, that is, he was removed from all ARV drugs and carefully monitored. So far, he has been disconnected from all HIV treatment, but has maintained a completely suppressed viral load for 65 weeks, according to sensitive tests. His last test was conducted on June 22, 2020.
The man's HIV antibody levels decreased after he started an intensive regimen, until he eventually returned to an HIV-negative state—which meant that the standard rapid HIV antibody test turned negative.
In his presentation of this case at the virtual AIDS conference, Diaz stressed that further tests are needed to identify the potential persistence of HIV in the Brazilian man's body, as well as longer follow-up before he and his colleagues can come to more definitive conclusions about the significance of this case.
In other words, only time will tell if the Brazilian man has really recovered.
During a teleconference held a week before the AIDS 2020 conference, Monica Gandhi, MD, from the University of California, San Francisco, stressed: “These are amazing results. But they are very preliminary. It happened to one person and only one person. We must observe the other participants in this important study.”
Despite all these qualities, Gandhi expressed admiration that the Brazilian did not need “something terrible like a bone marrow transplant” to achieve a state of prolonged viral remission.
Many people, including infants who started receiving ARV drugs very soon after contracting HIV and then stopped treatment for this virus, have maintained a completely suppressed virus for many years. Perhaps the most widely known cases are when it comes to an African child and a French teenager. A group of adults under the supervision of French researchers, known as the Visconti cohort, is also in viral remission, due to the very early initiation of ARV treatment.
However, the most famous such case ended in bitter disappointment.
In this case, the child, known as the ”Mississippi baby," contracted HIV from his mother and was put on an enhanced ARV regimen shortly after birth. The child made global headlines in 2013 after the first case study about her revealed that her virus had not recovered after she was taken off ARV therapy as a child. It was widely announced at the time that she was cured, or at least “functionally cured."- But in the end, 27 months after the termination of treatment, the girl had a viral rebound, and she was transferred back to ARV therapy.
After this bitter disappointment, researchers in the field of HIV treatment have become much more careful in choosing the words with which they characterize a person who does not experience a viral rebound for a long period after stopping HIV treatment.
“Even with a relatively long absence of antiretroviral drugs, we have to be very careful when interpreting the results and monitoring this patient," Diaz Pos said, referring to the Brazilian. “We must not forget that the child from Mississippi controlled [his] infection for a long time, but not for an indefinite time.”